Searching for a reliable way to assess mobility in elderly individuals? The process can be laden with uncertainty and concern.
Our Elderly Mobility Scale Calculator is a tool forged from professional expertise, tailored for individuals and caregivers alike, aiming to build a bridge of understanding and trust. In this article, we delve into how this calculator demystifies mobility assessment, facilitating a smoother journey towards improved quality of life for the elderly.
Elderly Mobility Scale Calculator
EMS Score:
What is the Elderly Mobility Scale (EMS)?
Definition
Due to technological influence, there are accessible ways to ensure that the health condition of the elderly is being monitored. The Elderly Mobility Scale (EMS) is a clinical tool used to assess the mobility and function of elderly individuals. According to the Chartered Society of Physiotherapy, the EMS is used for older people in a hospital setting, either in a day hospital or on a ward; its purpose is to provide a scale assessment for mobility while considering balance, locomotion, and key position changes.
Moreover, the whole EMS and the Functional Reach component can predict a risk of falling for an individual. Speaking of Functional Reach, this is one of the components for an EMS to function.
Components of the EMS
- Functional reach
- Sit-to-stand
- Walking speed
- Turning ability
- Stair climbing
1. Functional reach
This is a common component of mobility assessment scales, especially in evaluating stability and balance. This can assess an individual's dynamic balance and ability to reach forward without taking a step or losing balance.
2. Sit-to-stand
This component assesses the ability of an individual to transition to a standing position from a seated position, which can be a challenging but fundamental mobility task. Sit-to-stand is specifically designed to evaluate the lower limb strength of an individual, as well as their functional mobility and balance while getting up from a chair.
3. Walking speed
Walking speed provides valuable information about an older person's functional abilities. Walking speed assessment usually involves measuring the time it takes for an individual to walk a particular distance. This assessment offers insights into an individual's muscle strength, gait, balance, and overall mobility.
4. Turning ability
This can assess an individual's ability to switch direction while walking or transitioning between positions like pivoting, turning around, or making lateral movements.
5. Stair climbing
Stair climbing, as a common daily activity, involves coordination, endurance, strength, and balance. Assessing the ability of an individual to climb stairs can provide insights into their capacity to navigate different environments and their functional mobility.
How Does the Elderly Mobility Scale Calculator Work?
Scoring System
Take note that each component of the mobility scale corresponds to a specific task or mobility ability that an elderly individual is assigned to perform. There are pre-defined scoring criteria that outline the criteria and the range of possible scores for assigning such scores.
The scoring system assigns a numeric value to each component depending on an individual's performance. In general mobility cases, higher scores are associated with higher functional or better mobility, while lower scores show mobility difficulties or limitations.
After the assessment of components, the scores for all components are usually summed to calculate the total score on the mobility scale of an individual. Whatever the total score may be, this provides an overall measure of a person's functional ability and mobility.
The total score range can be divided into three parts: scores under 10, scores between 10-13, and scores over.
Under 10:
When scores are under 10, patients depend on mobility maneuvers, which require help with basic Activities of Daily Living (ADL) like toileting, dressing, and transfers.
Between 10-13:
Scores between 10-13 show that these patients are borderline regarding independence and safe mobility in ADL; they'll require some help with mobility maneuvers.
Over 14:
Lastly, if the scores are over 14, patients can perform mobility maneuvers alone and are independent and safe in basic ADL.
Using the Calculator
The following are steps in using the calculator for an Elderly Mobility Scale:
1. Gather Information
Gather the individual's necessary information, such as the individual's height, sex, age, and mobility assessment results.
2. Access the Calculator
A physical calculator provided by a healthcare family or an online calculator accessible online on a legitimate medical website.
3. Input Basic Information
Enter the individual's basic information, such as height, age, and sex.
4. Enter Component Scores
Input the scores obtained during the assessment for each component (ex., turning ability, walking speed, stair climbing) of the mobility scale. Depending on the scale, you may enter numeric scores, category selection, or a specific format.
5. Calculate Component Subtotals
Calculate the subtotals (ex., balance, lower limb strength, gait) for different components based on the scores entered from the scale's instructions.
6. Calculate the Total Score
Sum up the component subtotals or individual component scores using the calculator to calculate the total score for the elderly mobility assessment. The calculator will provide you with the final score.
7. Interpret the Total Score
In interpreting the total score, remember that higher scores show better mobility, while lower scores show greater mobility limitations.
8. Make Clinical Decisions
If applicable, use the category and total score to guide clinical decision-making. This can include rehabilitation plans, identifying interventions, and fall prevention strategies, depending on the mobility level of the individual.
9. Monitor Progress
Record the total score if you're using the calculator for tracking mobility over time, and use it as a reference for future assessments.
10. Document and Communicate
Document the total score and any relevant details in the patient's records. Communicate the findings and suggestions with the healthcare team, caregivers, and especially the individual to ensure cooperation and transparency in healthcare.
Benefits of Using the EMS Calculator
The EMS Calculator has several benefits in ensuring that caregivers or medical professionals adequately assess the mobility of elderly people. The EMS Calculator aims to provide early detection of mobility issues for timely interventions to prevent further decline.
The development of personalized care plans is crucial as it's tailored to an individual's specific mobility needs and limitations. Fall risk assessment is one of the well-known benefits of the EMS Calculator. Always note that lower scores can suggest a higher fall risk, allowing caregivers and medical professionals to implement fall prevention strategies.
Lastly, regular monitoring through repeated assessments can track changes in mobility over time. This benefit can help identify improvements, declines, and potential issues.
Scientific Studies and Data on EMS
Validity and Reliability
Past and ongoing studies continue to show that the Elderly Mobility Scale (EMS) is beneficial as an assessment tool for functionality and mobility for older people. A 2014 study demonstrated the effectiveness of EMS in linking a strong positive relationship between ADL (Activity of Daily Living), QOL (Quality of Life), and EM (Elderly Mobility) on older adults at a geriatric home at Makkah Al-Mukarramah. It was discovered that older people are entirely dependent on mobility and ADL.
Another study published in Wiley Online Library showed the effectiveness of the Elderly Mobility Scale (EMS) in 50 geriatric patients who were admitted to a medical ward in a Norway hospital. The original version of the Elderly Mobility Scale (EMS) was translated into Norwegian from English. Results showed that the EMS-N tool showed good internal consistency, criterion validity, and test-retest reliability.
In correlation with other mobility assessment tools, a 2008 study from the National Library of Medicine showed that instruments such as EMS (Elderly Mobility Scale), HABAM (Hierarchical Assessment of Balance and Mobility), and PPME (Physical Performance Mobility Examination) consist of methods such as balance and walking items, bed transfers, and chair transfers. But, the testing protocols, scoring systems, and wording can vary across instruments.
The EMS provides a three-point response option for patient independence for bed mobility tasks with transfers from lying to sitting and vice-versa. While HABAM provides a dichotomous response option independently for positions in bed, lying, and sitting. PPME can use either a two or three-option scoring system in assessing sitting up in bed (from lying down).
Recent Research Findings
Recent studies show only a few new modifications or improvements to EMS. However, recent studies on general elderly mobility continue to flourish. The Elderly Mobility Scale (EMS) was translated to Norwegian from English before initiating a 2020 study. Using the short physical performance battery (SPPB) as the gold standard, EMS-N (Elderly Mobility Scale-Norwegian) was tested for test-retest reliability, criterion validity, and internal consistency. Positive results were shown, making EMS-N a beneficial assessment tool for hospitalized geriatric patients.
In terms of outcomes on recent studies surrounding elderly mobility, a 2017 study under BMC Public Health showed that Mobility Over Varied Environments Scale (MOVES) is used as a holistic measure of mobility for older adult mobility characterization in a Canadian population.
This approach holds utility for surveillance, intervention, evaluation, and research around broad factors influencing mobility. This comprehensive elderly mobility approach is a complex inherent in mobility, including social, transportation, physical, and cognitive domains.
Practical Applications of the EMS Calculator
Clinical Settings
The Elderly Mobility Scale (EMS) is a crucial mobility assessment tool that can be comprehensive and flexible in practical applications. The EMS can help medical professionals in acute care hospital settings assess the mobility status of elderly patients who have been admitted for various medical injuries, conditions, and surgeries.
It also implements fall risk assessments for preventive measures and patient safety during hospitalization. Regarding rehabilitation centers, the EMS can tailor rehabilitation plans to address particular mobility deficits and develop individualized care plans to identify mobility limitation areas.
Lastly, EMS is used in nursing homes as a part of the admission assessment for new residents. This assessment provides patients with personalized care plans, provision of mobility aids, and fall prevention strategies.
Incorporating EMS in medical institutions is beneficial in enhancing the mobility and overall well-being of elderly individuals.
Home Assessments
Caregivers and family members can provide adequate care for the elderly by using the EMS at home. Before starting the assessment, make sure to prepare the needed materials, such as a sturdy chair, a flat surface for walking, any assistive devices like a walker or cane, and a stopwatch or timer.
Familiarize reviewing the EMS assessment items, which include walking, turning, sitting down or standing up from a chair, and other balance-related activities. Before performing the assessment, follow the instructions provided by medical professionals.
Assign a score based on the person's performance after completing the task, then record the assessment scores. Also develop a mobility plan with the help of a medical professional, which can include assistive devices and exercises for mobility improvement.
Share the results with a medical professional and continue conducting regular assessments, especially for those living alone. Regular assessments can prevent functional decline, fall prevention, and monitor mobility.
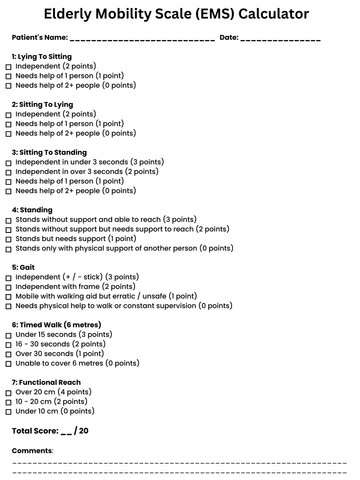
⬇️ Download Our Printable Elderly Mobility Scale Calculator ⬇️
Click the image or here to download the printable PDF version of our EMS Calculator.
Frequently Asked Questions (FAQs)
1: What is the difference between the EMS and other mobility scales?
An evident unique feature of the EMS is that it is made explicitly for elderly individuals as it assesses various aspects of mobility such as gait, transfers, functional mobility, and dynamic balance.
Compared to the Barthel Index, it evaluates activities of daily living (ADLs), including items related to mobility, but it doesn't give a comprehensive mobility assessment.
The Timed Up and Go Test (TUG) provides a general way to assess basic mobility, and it relies on the captured time to get the score instead of using a 20-point scale like the EMS.
On the other hand, the John Hopkins Highest Level of Mobility Scale (JH-HLM) is specifically designed for in-hospital use. According to the American Geriatrics Society, nurses rate patients the mobility they achieve on its highest level. This scale is only for hospital use, unlike the EMS, which can be done in the confines of your home.
2. How often should the EMS be administered?
The administration of the Elderly Mobility Scale (EMS) will always vary depending on the goals of care, clinical guidelines, recommendations of healthcare professionals, and the individual's health status and preferences. The EMS can be administered more frequently if the individual is undergoing rehabilitation in order to track progress.
3. Can the EMS predict the risk of falls in the elderly?
Implementing the EMS usually requires minimal training where its requirements include the educational background, continuing education (workshops), and certifications of caregivers, nurses, or geriatric specialists. Available resources can come from associations like the American Physical Therapy Association, peer-reviewed journals, healthcare professionals, and clinical guidelines from reputable sources such as the World Health Organization (WHO).
4. Are there any limitations to the EMS?
According to the Chartered Society of Physiotherapy, potential limitations can be evident in using the EMS. This can include difficulty in use in community environments and insensitivity for patients with poor confidence issues.
The scale, in some cases, can have floor or ceiling effects, which can limit the ability to differentiate between individuals with extreme mobility cases. Moreover, ethical and cultural considerations must be applied to provide comfort and security to the individual.
Conclusion
In conclusion, elderly mobility assessment is vital in monitoring cognitive and psychological health, early detection of health issues, fall prevention, and customized care planning for elderly people.
The Elderly Mobility Scale (EMS) provides a comprehensive evaluation in identifying mobility improvements and limitations. In ensuring optimal elderly care, caregivers and medical professionals must be encouraged to regularly use the EMS calculator for adequate progress tracking to monitor potential mobility issues that can occur, prevent fall risks, and promote good quality of life.